Sleep apnea, a prevalent yet frequently undiagnosed sleep disorder can profoundly affect one’s overall health. The condition is characterized by pauses in breathing during sleep, known as “apneas,” which disrupts the natural sleep cycle leading to fragmented sleep and a myriad of health issues. In this article, we will provide overview of sleep apnea, exploring its types, signs & symptom’s, risk factors and treatment options.
Types of Apneas
Obstructive Sleep Apnea (OSA)
OSA is the most prevalent type, characterized by the excessive relaxation of throat muscles during sleep. This relaxation causes a physical blockage of the upper airway, resulting in repeated disruptions in breathing. Pauses in breathing, often accompanied by loud snoring, contribute to fragmented sleep patterns.
Central Sleep Apnea (CSA)
Less common than OSA, CSA results from a malfunction in the brain’s respiratory control center. In CSA, the brain fails to send signals to the muscles responsible for breathing, leading to a lack of effort to breathe during sleep. Unlike OSA, which involves physical airway obstruction, CSA is characterized by pauses in airflow without accompanying efforts to breathe.
Complex Sleep Apnea Syndrome
Also known as treatment-emergent central sleep apnea, this type combines obstructive and central sleep apneas. It may develop in individuals using continuous positive airway pressure (CPAP) therapy for OSA. Careful monitoring and adjustment of treatment strategies are crucial for those experiencing complex sleep apnea syndrome.
Recognizing Signs & Symptoms
Sleep apnea manifests through various symptoms, including loud snoring, abrupt awakenings with shortness of breath, excessive daytime fatigue, difficulty concentrating, and morning headaches. Recognizing these signs is essential for timely intervention.
1.) Loud Snoring
Persistent and pronounced snoring is a telltale sign of OSA, stemming from the vibration of throat tissues as air battles through a constricted airway.
2.) Breath Holding & Pauses
Witnessed by a bed partner, these episodes indicate potential OSA, involving pauses in breathing accompanied by sudden gasps or choking sounds.
3.) Daytime Sleepiness & Fatigue
Fragmented sleep caused by OSA contributes to daytime sleepiness and fatigue. Exploring the connection between OSA and its impact on daily activities sheds light on the importance of timely diagnosis and intervention.
3.) Morning Headaches
Resulting from oxygen fluctuations during disrupted breathing, morning headaches underscore the potential health implications of untreated sleep apnea.
4.) Brain Fog & Difficulty Concentrating
OSA is associated with cognitive impairment, difficulty concentrating, and memory problems. Addressing cognitive challenges emphasizes the need for comprehensive sleep assessments.
5.) Irritability & Mood Changes
OSA contributes to irritability, mood swings, and heightened stress levels. Holistic approaches to sleep apnea management are crucial for emotional well-being.
6.) Dry Mouth & Sore Throat
When the upper airway collapses or becomes partially blocked, individuals with sleep apnea may unconsciously switch to breathing through their mouths, leading to decreased saliva production. This mouth breathing can result in dryness of the oral cavity and throat.
7.) Nighttime Urination
The stress response triggered by repeated episodes of interrupted breathing can lead to an increase in the production of certain hormones, such as atrial natriuretic peptide, promoting urine production. Additionally, the disruption of the normal sleep cycle and the resulting fragmented sleep can affect the body’s fluid balance, leading to an increased need to urinate during the night.
8.) Sexual Dysfunction
The intermittent oxygen deprivation and sleep fragmentation associated can affect hormone production, including testosterone, essential for sexual function. Chronic fatigue, a common consequence of untreated sleep apnea, can further contribute to diminished libido and sexual performance.
8.) High Blood Pressure
The temporary cessation of breathing leads to oxygen deprivation and triggers the body’s stress response, releasing hormones that increase heart rate and constrict blood vessels. Furthermore, the frequent awakenings disrupt the normal sleep cycle, contributing to a state of chronic stress also increases blood pressure. Over time, this can lead to the development or worsening of hypertension and increase risk of cardiovascular complications.
Risk Factors
Certain factors, such as obesity, family history, smoking, and medical conditions like hypertension and diabetes, increase the likelihood of developing sleep apnea. Recognizing these risk factors contributes to early detection and effective management.
Treatment Options
Lifestyle Modifications
Lifestyle modifications play a crucial role in managing sleep apnea. Weight loss through a balanced diet and regular exercise can reduce excess tissue contributing to airway obstruction. Avoiding alcohol and sedatives, especially before bedtime, helps prevent muscle relaxation in the throat. Sleeping on one’s side instead of the back can also alleviate airway constriction. Additionally, maintaining a consistent sleep schedule and creating a conducive sleep environment with minimal distractions contribute to improved sleep quality for individuals with sleep apnea. These lifestyle adjustments, when combined, can significantly enhance the effectiveness of overall sleep apnea management.
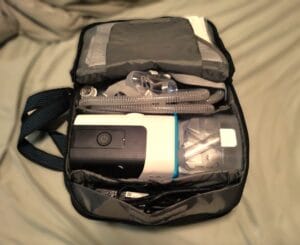
Continuous Positive Airway Pressure (CPAP)
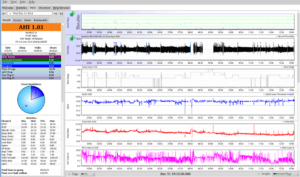
Continuous Positive Airway Pressure (CPAP) works by delivering a continuous stream of pressurized air through a mask worn over the nose or both the nose and mouth. This constant flow acts as a splint, preventing the collapse of the upper airway during sleep, which is a common issue in obstructive sleep apnea (OSA). By maintaining an open airway and eliminating breathing interruptions, CPAP therapy enhances oxygen saturation in the blood, improves sleep quality, and reduces the symptoms associated with OSA, such as loud snoring and daytime sleepiness. Consistent use of CPAP is crucial for long-term benefits and overall health improvement in individuals with sleep apnea. You can read more about these devises in our other article about Finding the Best CPAP Machine which provides comprehensive overview of considerations when choosing a machine.
BiPAP & Adaptive Servo-Ventilation
BiPAP (Bilevel Positive Airway Pressure) and Adaptive Servo-Ventilation (ASV) are advanced positive airway pressure therapies used to treat sleep disorders like sleep apnea. BiPAP provides two distinct pressure levels – higher pressure during inhalation and lower pressure during exhalation – offering more customized respiratory support compared to CPAP. ASV, on the other hand, adjusts air pressure based on the individual’s breathing patterns, providing a tailored response to variations in respiratory effort. Both BiPAP and ASV are alternatives for individuals who may not tolerate standard CPAP therapy, offering flexibility and improved comfort in the management of sleep-related breathing disorders.
Surgical Procedures
Surgical procedures for sleep apnea aim to alleviate airway obstruction and improve breathing during sleep. Common surgeries include Uvulopalatopharyngoplasty (UPPP), Genioglossus Advancement (GA), Maxillomandibular Advancement (MMA), and others targeting specific anatomical issues. These interventions are considered when non-surgical treatments like CPAP are ineffective or not well-tolerated. Each surgery addresses different aspects of airway obstruction, and the choice depends on the patient’s individual condition and anatomy. Consultation with a sleep specialist and otolaryngologist is essential to determine the most suitable surgical approach.
Final Thoughts
Understanding sleep apnea is the first step toward effective management and improved quality of life. If you suspect sleep apnea, seeking guidance from healthcare professionals is crucial. By unraveling the causes, recognizing symptoms, and exploring treatment options, individuals can reclaim restful nights and embrace a healthier, more energized lifestyle. Remember, a good night’s sleep is not just a luxury; it’s a necessity for overall well-being.